It started with a toy organ and a relative’s birthday celebration.
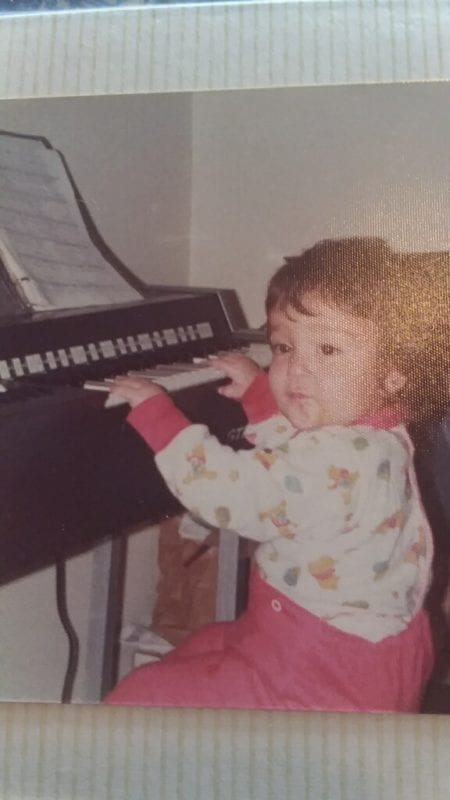
Sherrye Platt, at left, was three years old when she sat at her family’s toy organ and played the Happy Birthday tune without any instruction. Music became a lifelong hobby and eventually a fulfilling career as a board-certified music therapist. While an undergraduate at Montclair State University (MSU), where she studied to be a music teacher and eventually earned her bachelor’s, Platt was introduced to music as an evidence-based therapeutic tool being leveraged across disciples including mental health, military populations, trauma victims, and those afflicted with neurological conditions like Parkinson’s and Alzheimer’s. Platt quickly re-focused her studies to leverage the power of music to improve people’s lives. “Music helps with confidence, the ability to process difficult life experiences and anxieties as well as tackle insecurities,” she said, “it can calm agitation, provide a rhythm during a physical therapy visit and, most importantly, bring joy, which is more important now than ever. Therapeutic music is a relevant clinical tool that can complement all healthcare disciplines. I knew it was where I belonged, helping people rather than teaching them.”
Platt first applied her music therapy knowledge in an assisted living community where she specialized in patients with memory impairments. Because much of this population was elderly, end-of-life applications became a natural progression in her work. She began applying the neutrality of music to bridge the gap for patients and families during the death process, uniting them during what can feel like an unnatural time for many. After a decade devoted to one facility, Platt wanted to apply the benefits that music therapy brings at end of life exclusively to those in hospice care. She joined RVNAhealth in June 2020 at the height of the COVID-19 pandemic.
Hired to support the ComfortWELL hospice population and their families, Platt feels honored to be with patients and their loved ones at the end of their journey together and is privileged to provide a tool that brings families together. “Loved ones often don’t know what to say or how to interact with someone who is actively dying,” she said, “and hearing is believed to be the last of the senses affected in the death process, so music can be healing and unifying during a sacred, but difficult time.” Platt works closely with RVNAhealth Hospice Volunteer Coordinator, Stephanie Notaro and the two developed a professional affiliation with MSU to mentor music therapy undergraduate students. The alliance is mutually beneficial because patients benefit from young minds applying fresh ideas, to which Platt herself might otherwise not be exposed, and the students have direct patient contact introducing them to the complexities of individual need. Some hospice patients respond to upbeat, fast tempo music whereas others prefer a quieter backdrop. Of course, this can change from session to session, so intuition and training are important factors for the specialty.
A music therapy education is quite comprehensive and encompasses more than just musical skill. Platt earned her master’s degree at world-renowned Berklee College of Music and noted that, “music is not the goal, rather the method used to reach it.” The certification preparation includes developing counseling knowledge and skill as well as neuroscience expertise to best understand the brain/body response. The comprehensive care offered by RVNAhealth was particularly appealing to Platt because the music therapy discipline is not stand alone and can benefit all services that the organization offers. “Music therapy can help social work and pastoral care with emotional, spiritual and familial objectives as well as nursing for things like pain management and agitation. It’s a complementary therapy that can be utilized to achieve so many different goals,” she said.
Recently, Platt has been using her ukulele instead of the guitar at patient bedsides, particularly those succumbing to COVID-19 because the demure sound allows her to get as close to the patient as safely possible. “It’s tough being surrounded by people in full [PPE] garb because it removes that closeness. I can overcome that barrier using the ukulele; it is such a pure sound that brings out vulnerability and pure emotion. It is a great honor to use music to help people feel things they otherwise might not. Every day is a privilege.”
To explore how music therapy can benefit your patients, contact RVNAhealth at 203-438-5555 or intake@rvnahealth.org.